FSHD Symptoms & Patient Experiences
What are symptoms of FSHD?
Facioscapulohumeral muscular dystrophy (FSHD) is a type of neuromuscular disease (NMD) that affects both men and women. Like other forms of muscular dystrophy, it causes muscles to weaken over time, making everyday movements harder.
FSHD often begins to show in teens and young adults, though every person’s journey is different. Some start noticing symptoms as early as childhood, while others may not realize they have FSHD until much later in life. In fact, about 5% of people with FSHD develop symptoms before age 10, while some seniors have such mild symptoms that they go undiagnosed for years.
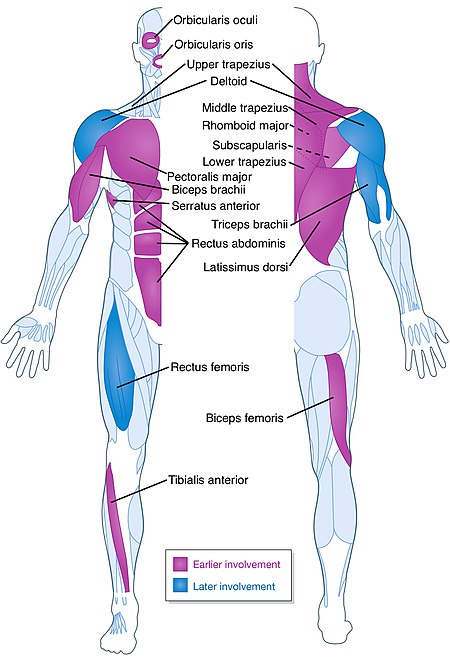
FSHD gets its name because it mainly affects the muscles in the face (facio), shoulders (scapula), and upper arms (humeral). However, it can also weaken other muscles, like those in the stomach, hips, and legs. One unusual thing about FSHD is that it doesn’t affect all muscles at the same time or in the same way. A muscle may get weak while the ones next to it stay strong. Later, a different muscle might be affected. This happens in an unpredictable way, which is why FSHD often causes uneven weakness, such as in just one arm or one leg.
At first, symptoms might seem like an injury, and it may take many people years before a doctor can make the right diagnosis.

Common symptoms can include:
- Trouble whistling
- Hard time sipping through a straw
- Eyes that don’t fully close during sleep
- Difficulty doing sit-ups and pull-ups
- Shoulder blades that stick out (winging)
- Trouble lifting arms above shoulder height
- Weakness in hands and fingers
- Foot drop (trouble lifting the foot)
- Weak stomach muscles, causing a “pregnant” belly look
- Loss of chest muscles
- Sunken chest (pectus excavatum)
- Curved spine (lordosis, kyphosis, scoliosis)
- Chronic tiredness (fatigue)
- Pain, sometimes severe (happens in 70% of people with FSHD)
People with FSHD may also have:
- Episodes of feeling really tired or muscle pain that feels like burning
- Sudden falls when their legs unexpectedly give out
- Trouble breathing
- Hearing loss
- Coats’ disease (an eye condition that is rare—see Early Onset FSHD for more info)
- Mild heart rhythm problems (happens in 5-9% of people)
At first, these symptoms might be missed or mistaken for an injury. Since many doctors don’t know much about FSHD, it can take a long time—an average of 9 years—to get the right diagnosis. Pain and tiredness can make daily life harder, even though people don’t always realize how much they affect someone with FSHD.
Losing facial expressions, having trouble moving, and feeling like others don’t understand can be emotionally tough, leading some people to pull away from social activities. Finding a good support system can make a big difference. That’s why the FSHD Society encourages people to join a local chapter or connect with online groups where they can share their experiences and learn from others.
Watch and share our "FSHD 101" video to learn more:
References:
- 1 Leung DG. Magnetic resonance imaging patterns of muscle involvement in genetic muscle diseases: a systematic review. J Neurol. 2016 Nov 25;264(7):1320–33.
- 2 Tasca G, Monforte M, Iannaccone E, Laschena F, Ottaviani P, Leoncini E, et al. Upper Girdle Imaging in Facioscapulohumeral Muscular Dystrophy. Martelli F, editor. PLoS ONE. 2014 Jun 16;9(6):e100292–11.
- 3 Regula JU, Jestaedt L, Jende F, Bartsch A, Meinck HM, Weber MA. Clinical Muscle Testing Compared with Whole-Body Magnetic Resonance Imaging in Facio-scapulo-humeral Muscular Dystrophy. Clin Neuroradiol. 2015 Apr 10;26(4):445–55.
- 4 Tasca G, Monforte M, Ottaviani P, Pelliccioni M, Frusciante R, Laschena F, et al. Magnetic resonance imaging in a large cohort of facioscapulohumeral muscular dystrophy patients: Pattern refinement and implications for clinical trials. Ann Neurol. 2016 Apr 4;79(5):854–64.
Additional information
- Download our brochure About FSHD (Download in Spanish)
- Download our Physical Therapy and FSHD brochure
- Diagnosis
- Genetic testing
- Early-onset FSHD
Clinical descriptions of symptoms
“Generally, FSHD displays a characteristic gradual spread of muscle involvement, starting in the face and slowly progressing to the shoulder and upper-arm musculature and to the abdominal and foot-extensor muscles” (1). “Foot dorsiflexion weakness leading to footdrop is an early manifestation of FSHD and one amenable to the use of molded ankle-foot orthoses (AFO)” (2). “The most common initial symptom is difficulty reaching above shoulder level. Less common presentations include foot drop (such patients, however, almost invariably have compensated), asymptomatic scapular fixator, and facial weakness on examination. Truncal weakness is an early and frequent manifestation that is easily overlooked during examination of these patients. Weak abdominal muscles result in a protuberant abdomen and contribute to the lumbar lordosis. Lower abdominal muscles are weaker than the upper abdominal muscles, causing a strikingly positive Beevor’s sign, a physical finding fairly specific for FSHD” (2). “Associated non-skeletal muscle manifestations include high-frequency hearing loss as well as retinal telangiectasias, both of which are rarely symptomatic” (2). “Approximately half of the patients present with subclinical high-tone hearing loss and retinovasculopathy” (1). Respiratory involvement in FSHD is not typical but can be seen, especially in patients with severe FSHD. Symptoms and signs of respiratory insufficiency should be sought during routine clinic visits in patients with severe FSHD, and regular monitoring of respiratory function instituted. “Symptomatic respiratory insufficiency can be initially managed with nighttime noninvasive pressure support (BiPAP) but may in severe cases require the use of a ventilator” (2).
1. van der Maarel SM, Frants RR. The D4Z4 repeat-mediated pathogenesis of facioscapulohumeral muscular dystrophy. Am J Hum Genet. 2005 Mar; 76(3):375-86. Review.
2. Tawil R, van der Maarel SM. “Facioscapulohumeral muscular dystrophy.” Muscle Nerve. 2006 Jul; 34(1):1-15. Review..
Other medical terms for FSHD
- Landouzy-Dejerine Muscular Dystrophy—The previous name for FSHD, named after Landouzy and Dejerine, who first described the disease in 1885.
- Facioscapulohumeral Disease—The term used by Dr. George W.A.M. Padberg in 1980 to describe FSHD as a multi-system, whole body disease.
- Facio-Scapulo-Humeral Muscular Dystrophy—A less common variation of the spelling of facioscapulohumeral muscular dystrophy.
- Fascioscapuohumeral Muscular Dystrophy—A less common spelling alternative for FSHD.
- Scapulohumeral Muscular Dystrophy—A facial-sparing form of dystrophy whose genetic locus may be the same as that for FSHD. There is no demonstrable facial weakness in affected individuals.
- Coats’ Disease—Also called retinal telangiectasis, a disorder characterized by a defect of retinal vascular development that results in vessel leakage, subretinal exudation, and retinal detachment. The disorder was first reported by Coats in 1908. It is usually associated with infantile or early-onset FSHD.
- Bilateral Sensorineural Hearing Loss—A high-frequency hearing loss caused by nerve damage in both ears. Usually associated with and clinically symptomatic in infantile or early-onset FSHD.
- Hypercarbic Respiratory Insufficiency—Respiratory insufficiency caused by high levels of carbon dioxide (CO2) in the blood.
