Is this the ticket to gene therapy for muscle diseases?
by June Kinoshita, Director of Research and Patient Engagement

A lot of emails cross my desk every day, but one that came last September from an FSHD patient pulled me right down a rabbit hole that proved to be fantastic. It was a story from the famous Harvard-MIT Broad Institute in Cambridge, MA, about a researcher who had harnessed a method called “directed evolution” to engineer special viruses that improved the efficiency of targeting gene therapies to skeletal muscle while limiting liver exposure, thereby reducing the toxic side effects frequently reported in gene therapy trials. Not only was the research a tour de force, but the scientist leading the charge, Sharif Tabebordbar, was inspired by his father’s battle with an unspecified “rare genetic muscle disease.”
Current gene therapy relies on a family of viruses called adeno-associated virus-9 (AAV9), which are adept at getting into cells to deliver the therapeutic “genetic fix.” However, one of the limitations of AAV9 is the non-specific delivery to different cell types. To treat diseases of muscle—which make up 40 percent of the body—one needs to inject enormous amounts of AAV9, but most of the virus end up not in muscle but in the liver, where it can reach dangerous levels. Some gene therapy trials had to be halted following patients’ deaths from liver damage. To address this shortcoming, many groups have sought to improve the efficiency of muscle delivery by testing different AAV9 sub-types. Although some improvements have been gained, liver exposure using these methods have only shown marginal benefits and toxicity remains a major concern.
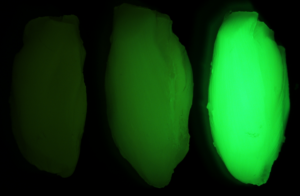
To solve this problem, Tabebordbar embarked on a bold experiment to alter the virus’s outer protein coat, called the capsid, so that it prefers muscle and avoids the liver. He and his team added random amino acids to the part of the AAV9 capsid that binds to cells. They made millions of varieties, injected them into mice and monkeys and isolated the ones that successfully entered and delivered therapeutic genes to muscle cells. They called this muscle-fancying virus MyoAAV.
Next, working with Alan Beggs of Boston Children’s Hospital, Tabebordbar’s team tested MyoAAV in mouse models of a genetic disease called X-linked myotubular myopathy (XLMTM), which is usually fatal in childhood. In his NIH director’s blog, Francis Collins described what happened. “The XLMTM mice normally die in 10 weeks. But, after receiving MyoAAV carrying a corrective gene, all six mice had a normal lifespan. By comparison, mice treated in the same way with traditional AAV9 lived only up to 21 weeks of age. What’s more, the researchers used MyoAAV at a dose 100 times lower than that currently used in clinical trials.”
Additional experiments showed that MyoAAVs also work in human muscle cells in a lab dish. These results, published in the top-line journal Cell, combined with the compelling personal story, garnered a glowing profile in the New York Times.
Excited by the research and curious to know more about the back story, we reached out directly to Tabebordbar. He told us his father’s mysterious ailment was indeed FSHD. He recalled growing up in Iran, how his father started to have problems with his balance. How the weakness spread through his body until he could no longer walk unaided. Today he needs a wheelchair and must use one hand to lift the other—a gesture familiar to many who share this diagnosis.
“I watched my dad get worse and worse each day,” Tabebordbar recalled. “It was a huge challenge to do things together as a family – genetic disease is a burden on not only patients but families. I thought: This is very unfair to patients and there’s got to be a way to fix this.”
We inquired whether Tabebordbar knew whether he had inherited FSHD from his father. He said he had himself tested and learned that, in a most unlikely reshuffling of the genetic deck, he had inherited the shortened D4Z4 region but not the “permissive” polyA section that is needed to stabilize the DUX4 messenger RNA. “Lucky” would be a vast understatement of how he dodged having FSHD himself.
What happens next? Tabebordbar said he hopes to develop gene therapies for a variety of muscle diseases. Should FSHD be one of the diseases chosen, we discussed how the FSHD Society can support these efforts, by pushing for validation of biomarkers and clinical outcomes for gene therapy clinical trials, engaging patients and families on the design of future trials and continuing our investment in the FSHD Clinical Trial Research Network.
The impact of Tabebordbar’s work may reach far beyond muscle diseases, as the directed evolution approach could in principle be used to generate AAVs with preferences for other organs in the body. “With this latest advance,” said NIH’s Francis Collins, “the hope is that the next generation of promising gene therapies might soon make its way to the clinic to help Tabebordbar’s father and so many other people.”
Reference
Directed evolution of a family of AAV capsid variants enabling potent muscle-directed gene delivery across species. Tabebordbar M, Lagerborg KA, Stanton A, King EM, Ye S, Tellez L, Krunnfusz A, Tavakoli S, Widrick JJ, Messemer KA, Troiano EC, Moghadaszadeh B, Peacker BL, Leacock KA, Horwitz N, Beggs AH, Wagers AJ, Sabeti PC. Cell. 2021 Sep 4:S0092-8674(21)01002-3.
Further reading
He Can’t Cure His Dad. But a Scientist’s Research May Help Everyone Else (NY Times)
Engineering a Better Way to Deliver Therapeutic Genes to Muscles (NIH)
A new gene-delivery vehicle could make gene therapy for muscle diseases safer and more effective (Broad Institute)


“What’s more, the researchers used MyoAAV at a dose 100 times lower than that currently used in clinical trials.”
Can that be expanded, please? That doesn’t sound like a positive except other than perhaps that the recipient is a mouse.
“We inquired whether Tabebordbar knew whether he had inherited FSHD from his father. He said he had himself tested and learned that, in a most unlikely reshuffling of the genetic deck, he had inherited the shortened D4Z4 region but not the “permissive” polyA section that is needed to stabilize the DUX4 messenger RNA. ”
Very interesting as my understanding is that we receive an entire chromosome from each parent. Would this be considered a mutation or is this considered a part of the normal genetic inheritance process?
Good questions. The point about the lower dose (this is adjusted for body weight) is that with a 100 times lower does, the researchers were still able to achieve high transfection rates in the muscle cells. A lower dose means a lower risk of toxic side effects. And also a lower cost for the therapy. Manufacturing gene therapies is a very expensive undertaking so the less material needed, the lower the cost should be.
Regarding the genetic “shuffling of the deck,” this type of genetic rearrangement is not uncommon. Even though we inherit one chromosome from each parent, pieces of genetic material can get moved around.
I was more referring to the statement about the liver toxicity of traditional AAV delivery systems of:
“Some gene therapy trials had to be halted following patients’ deaths from liver damage.”
With reference to the treatment delivery’s potential toxicity, using a lower does than typically used in trials didn’t sound confidence building. However, if using a significantly lower dose produces therapeutic effects, while in addition modifying the delivery system to further limit or even eliminate liver damage, then I see the position of the article.
Thanks for the response. I believe I’m now following the research better.
Another “breakthrough” that has zero relevance to the time frame of the lives of those who currently suffer from fshd. These breakthroughs always sound like finally this is the thing that will have some impact on my life. Reality is that the way the system works decades and lifetimes will pass before anyone with fshd is helped by this if at all.
We don’t think it’s “the system” that is at fault. Blame Nature. The genetics of FSHD was a super hard nut to crack. Working out what happens when muscles degenerate is proving to be equally challenging, if not more. Developing a version of AAV9 that targets muscle cells was made possible by the technological revolutions that led to directed evolution experiments. When compared to progress in major diseases like Alzheimer’s and cancer, FSHD has made remarkably rapid progress. Of course, it’s never fast enough for patients living with FSHD, and we agonize over this every day, but stepping back to look objectively at what is going on, we feel great hope.
Clearly the lack of urgency in the system is why losmapimod is in some state of limbo right now. Why does it take the better part of a year to work out with the FDA the next steps?
With regards to MYOAAV specifically, I discussed with researchers developing gene therapies for FSHD. They say this vector is still very hard on the heart and liver and will take the better part of a year to do a study in their own lab to see for themselves. I don’t understand this on many levels and surely not from the point of view from someone devastated by this disease that needs a therapy ASAP.
1. Yes, there has been problems caused by organ damage from viral vectors in some gene therapy studies especially those where the disease itself compromises the liver, but for example, current DMD trials using current vectors show acceptable tolerance with viral loads 100 times the claimed requirement using the MYOAAV vectors. So how is MYOAAV not a no brainer for muscle gene therapies? Why more delay to do more and more studies on something already studied thoroughly.
2. Why are FSHD people doing these independent studies when this vector applies to many neuromuscular diseases? It appears, at least on paper that there is an effort to dramatically reduce the bureaucratic overhead and inefficiencies in developing the viral vector part of gene therapies but I see no participation from FSHD advocacy or research. See next paragraph.
I am not sure why FSHD people seem to not be aware of the Bespoke Gene Therapy Consortium. https://directorsblog.nih.gov/tag/aav-mediated-gene-delivery/ I would hope MYOAAV vectors are a significant focus of this since DMD people are signatories. I hope this will not be just another glacially slow bureaucratic monster that sucks up precious time and resources and not dramatically fix this core systemic and frankly ridiculous inefficiency of duplication of efforts with gene therapy viral vectors.
In any case, gene therapy for FSHD, from I have heard from researchers, at least with current approaches and attitudes, will be many many years away MYOAAV or not. A significant part of this time is not because of the lack of technology it is because of inefficiencies in the process and the “oh well that’s just the way we do it” attitude. Maybe Bespoke fixes some of this for viral vectored gene therapies.
With FSHD there are several approaches to silencing DUX4 developed and tested in vitro in labs. And that’s great that we are looking for more approaches to silence DUX4 and are looking for other targets, but why not really strip away all the bureaucracy, duplication of efforts and the nonsensical “that’s just how things are done” delays in the translation to full access processes and take as many shots on goal with approaches already identified in the absolute shortest amount of time. (similar to Covid-19 vaccine approach instead of normal virus vaccine approach). You have to look no further than the limbo status of losmapimod to see a nonsensical delay. Future trials will have the same or worse nonsensical delays.
I have many genetic relatives with this and most of them are barely affected by it or have barely any symptoms even at an advanced age. I think that’s weird and I wonder if people in my family could be a source of a treatment for it or others that are minorly affected and mostly healthy.
Researchers are looking for families like yours to study. If you’re interested, please email june.kinoshita@fshdsociety.org.